Cache Coherence Protocols: MESI and MOESI Explained
TL;DR: AI is transforming drug discovery by designing molecules for previously untreatable diseases in months instead of years. Companies like Insilico Medicine and Isomorphic Labs already have AI-designed drugs in human trials, targeting rare diseases and conditions that traditional chemistry couldn't solve.

Within five years, you'll likely encounter a drug that was never touched by human hands during its design phase. Not because pharmaceutical companies laid off their chemists, but because artificial intelligence figured out molecular combinations that no human would have thought to test. The untreatable is becoming treatable, not through harder work or bigger budgets, but through machines that can explore chemical possibilities at a speed that makes traditional drug discovery look like searching for a needle in a haystack while blindfolded.
This isn't science fiction anymore. In early 2025, Insilico Medicine reported positive Phase I trial results for ISM5411, a drug designed entirely by generative AI to treat inflammatory bowel disease. Meanwhile, Isomorphic Labs is preparing its first human trials for AI-designed molecules targeting previously intractable diseases. These aren't incremental improvements. They represent a fundamental shift in how we approach the oldest challenge in medicine: turning theoretical cures into actual treatments.
For decades, drug discovery moved at a glacial pace. Developing a single drug took 10-15 years and cost billions of dollars, with a 90% failure rate. The problem wasn't lack of effort but pure mathematics. There are more possible drug-like molecules than there are atoms in the observable universe. Testing them all would take longer than the age of our solar system.
Then DeepMind's AlphaFold cracked protein folding, a problem that had stumped biologists for 50 years. AlphaFold 3, released in May 2024, can predict how proteins interact with DNA, RNA, and various molecules with 50% better accuracy than previous methods. That might sound incremental, but it's like going from a blurry photograph to HD video. Suddenly, researchers could see exactly how potential drugs would bind to their targets before synthesizing a single molecule.
What makes this revolutionary isn't just speed. It's the ability to explore chemical space that humans would never consider. Traditional drug discovery relies on chemists' intuition, tweaking known molecules to create better versions. AI doesn't have intuition or bias. It evaluates millions of molecular configurations based purely on predicted properties, uncovering compounds that work through mechanisms no one anticipated.
At its core, AI drug discovery combines three breakthroughs: deep learning for pattern recognition, generative models for creating new molecules, and reinforcement learning for optimization.
Deep learning models train on massive databases of known molecular structures and their properties. They learn the hidden rules governing how molecular shape determines function, which bonds are stable, which structures are toxic, and which configurations can actually be synthesized in a lab. This isn't memorization but pattern extraction at a scale impossible for human chemists.
Generative models, similar to those creating AI art or text, then design entirely new molecules. Instead of pixels or words, they arrange atoms and bonds to create structures predicted to have desired properties. Recent advances in generative AI allow these models to optimize for multiple goals simultaneously: potency against a disease target, low toxicity, ease of manufacturing, and even patient convenience like oral availability instead of injection.
The real magic happens with reinforcement learning. The AI proposes a molecule, receives feedback on its predicted properties, and iterates. This cycle repeats millions of times, exploring chemical space far beyond what any research team could attempt. Companies like Atomwise use this approach to screen billions of molecular combinations in days rather than years, identifying promising candidates that human chemists then synthesize and test.
The pharmaceutical industry has seen plenty of overhyped technologies fade into obscurity. AI drug discovery is different because it's already producing results that matter.
Insilico Medicine's ISM5411 represents the first wave of AI-designed drugs reaching human trials. Designed in under 18 months for inflammatory bowel disease, it targets a novel pathway that traditional approaches missed. Phase I trials showed it was safe and well-tolerated, a crucial first hurdle that validates the entire AI design process.

Rare diseases are seeing particularly dramatic benefits. These conditions affect too few patients for traditional drug development economics to work, leaving millions without treatment options. AI has enabled drug repurposing at scale, identifying existing approved drugs that could treat rare conditions they were never designed for. One AI system recently found a treatment for a rare genetic disorder by analyzing how the disease's molecular signature matched existing drug effects, a connection human researchers had missed for decades.
Isomorphic Labs, spun off from DeepMind, is pursuing what its CEO calls "solving all diseases" through AI. That's obviously hyperbole, but their pipeline includes molecules targeting conditions that pharmaceutical companies previously abandoned as too difficult. They're not just designing drugs faster; they're attempting diseases that were considered undruggable.
The technology is also accelerating drug discovery for conditions like Alzheimer's and cancer, where complexity has historically stymied progress. By predicting how molecules interact with multiple proteins simultaneously, AI can design drugs that target disease networks rather than single pathways, potentially overcoming the resistance that dooms many cancer treatments.
Every technological leap in medicine triggers familiar patterns of hope and skepticism. When sequencing the human genome became possible, optimists predicted personalized medicine within a decade. Twenty years later, genomics has transformed research but individual treatment remains limited for most patients.
The printing press didn't make everyone literate overnight, but it made literacy accessible in ways that eventually transformed civilization. Similarly, AI won't cure every disease immediately, but it's removing barriers that kept entire categories of treatments out of reach.
What's different this time is the feedback loop. Genomics was largely observational, revealing information without necessarily providing solutions. AI drug discovery is generative. It doesn't just analyze what exists; it creates what doesn't, guided by the same data that makes genomics powerful. We're combining the observational power of modern biology with the creative potential of computational design.
Previous drug discovery revolutions also required new infrastructure. High-throughput screening in the 1990s needed robotic systems and miniaturized assays. Biologics needed entirely new manufacturing processes. AI drug discovery needs massive computing power and curated datasets, but those prerequisites are getting cheaper and more accessible, not more expensive and rare.
Some disease targets were labeled undruggable not because we didn't understand them, but because traditional chemistry couldn't create molecules that would work. Protein-protein interactions, for example, involve large, flat surfaces where small drug molecules struggle to bind effectively.
AI is tackling these challenges by designing molecules with unconventional shapes and properties. Instead of the small, rigid structures that dominate traditional drugs, AI can propose larger, more flexible molecules that wrap around challenging targets like a custom glove. It can also predict which modifications make these molecules stable enough to survive in the human body without being immediately broken down.
Another category of undruggable targets involves proteins that lack clear binding pockets where drugs can attach. AI models trained on protein dynamics, not just static structures, can identify transient pockets that appear briefly during protein motion. Designing drugs that exploit these fleeting opportunities requires predicting molecular behavior across microseconds, a task far beyond human capabilities but well-suited to computational models.
The blood-brain barrier has historically blocked treatments for neurological conditions. Generative AI can now design molecules that are predicted to cross this barrier while maintaining their therapeutic effects, opening possibilities for treating conditions like Parkinson's and brain tumors that were largely inaccessible to traditional small-molecule drugs.
The pharmaceutical industry operates on blockbuster economics: a handful of successful drugs subsidize hundreds of failures. If AI reduces the failure rate from 90% to even 80%, the financial implications are staggering. Lower development costs could make rare disease drugs economically viable and reduce pressure for ever-higher drug prices.
But that's the optimistic scenario. The pessimistic one is that AI becomes another tool for consolidating power among companies that can afford the computational infrastructure and proprietary datasets. The cost of training cutting-edge AI models is already measured in tens of millions of dollars, creating barriers that smaller biotech companies struggle to overcome.

There's also the question of intellectual property. Can you patent a molecule that was autonomously designed by an AI? Current law says patents require human inventorship, but that's being tested as AI-designed drugs move through regulatory approval. The answer will determine whether AI drug discovery leads to more competition or greater monopolization.
Healthcare systems will also face adjustment. If AI enables hundreds of new treatments for previously neglected conditions, who decides which ones get funded? The technology might create abundance in drug candidates while exposing scarcity in healthcare budgets and regulatory capacity.
Faster drug development is valuable, but it's not the most important benefit. AI enables precision that was previously impossible.
Traditional drug development is essentially educated guessing. You design a molecule, synthesize it, test it, and repeat until something works. AI inverts this process. You specify the properties you want, and the algorithm designs molecules predicted to have them. This means you can optimize for patient-relevant factors from the start: once-daily dosing instead of three times daily, oral pills instead of injections, minimal side effects for specific populations like pregnant women or elderly patients.
AI also excels at finding unexpected connections. By analyzing thousands of diseases and millions of molecular interactions simultaneously, it can identify drug candidates that treat multiple conditions or repurpose existing drugs for new uses. This is already happening with rare diseases, but the same principle applies broadly. Your diabetes drug might turn out to be effective against certain cancers, a connection that emerges from computational analysis rather than serendipity.
The technology is also democratizing drug discovery. Academic researchers, who traditionally lack resources for extensive drug screening, can now use AI tools to identify promising candidates before approaching pharmaceutical partners. This could shift more control to researchers focused on specific diseases rather than commercial considerations.
For all its promise, AI drug discovery faces significant hurdles that enthusiasts often downplay.
Data quality remains a critical bottleneck. AI models are only as good as their training data, and pharmaceutical datasets are notoriously messy. Experiments conducted in different labs with different protocols produce incomparable results. Negative results, which are scientifically valuable, are rarely published. AI trained on this data can learn and amplify these biases, potentially designing molecules that look good in silico but fail in reality.
Regulatory agencies are struggling to adapt. How do you validate a drug designed by a process that even its creators don't fully understand? Deep learning models are black boxes, making predictions without explaining their reasoning. Regulators traditionally want to understand mechanism of action, but if the AI can't explain why a molecule should work, how do you assess safety?
There's also the clinical trial problem. AI might design better drug candidates, but it doesn't make clinical trials faster or cheaper. You still need to test safety in hundreds of patients, efficacy in thousands, and long-term effects over years. No algorithm changes that fundamental requirement, so the overall timeline from concept to pharmacy won't shrink as dramatically as the design phase alone.
Equity concerns are real. If AI-designed drugs are initially more expensive or available only in wealthy countries, we could see widening health disparities even as overall capability increases. The technology to design global health solutions exists, but the economic incentives might not align.
Within a decade, you'll likely benefit from AI-designed medicine without knowing it. The label won't say "designed by artificial intelligence," just the drug name and dosage. But the impact will be profound.
Rare disease patients, who currently face a lottery of whether their condition is profitable enough for drug development, could see their odds improve dramatically. Cancer patients might receive treatments designed specifically for their tumor's genetic profile, not just their cancer type. Antibiotic resistance, one of the gravest threats to modern medicine, could be countered by AI systems that design new antibiotics faster than bacteria evolve resistance.
The shift also changes medical research priorities. If designing drug candidates becomes cheaper and faster, research bottlenecks move elsewhere: patient recruitment for trials, manufacturing scale-up, regulatory review, and healthcare system adoption. These are all fundamentally human processes that don't accelerate just because the underlying science does.
Society will need to grapple with questions about access and control. Who owns the AI models that discover life-saving drugs? Should they be open source, or does proprietary development drive faster innovation? How do we ensure that AI-designed treatments reach patients in low-income countries, not just wealthy markets?
If you're a patient with a currently untreatable condition, the most important thing to understand is that "untreatable" is becoming a temporary label rather than a permanent one. Clinical trials for AI-designed drugs are expanding, and patient advocacy groups are increasingly aware of these opportunities.
For healthcare professionals, the change is more immediate. Understanding how AI-designed drugs differ from traditional ones, including their optimization criteria and potential failure modes, will become essential. The doctors of 2030 won't need to understand transformer architectures, but they'll need to interpret clinical data on drugs designed through fundamentally different processes.
The broader public should develop literacy in what AI can and can't do. It's not magic, and it won't cure everything. But it is a genuine capability expansion that will reshape medicine in ways we're only beginning to understand. The question isn't whether AI will transform drug discovery, that's already happening. The question is whether we'll guide that transformation toward equity and broad benefit, or allow it to amplify existing disparities.
The most exciting aspect isn't any single breakthrough but the trajectory. Each AI-designed drug that succeeds validates and improves the models, creating a positive feedback loop. The algorithms that designed today's clinical trial candidates are already obsolete, replaced by versions trained on more data and better architectures. We're not approaching a plateau; we're still in the early exponential phase.
The diseases we currently consider untreatable aren't scientifically impossible to cure. They're mathematically impractical for humans to solve alone. By offloading the combinatorial explosion of drug design to machines that excel at exactly that kind of problem, we're not replacing human ingenuity. We're augmenting it in ways that expand what's medically possible. The question isn't whether this will work. It already is. The question is how fast we can scale it, and who benefits as we do.

Ahuna Mons on dwarf planet Ceres is the solar system's only confirmed cryovolcano in the asteroid belt - a mountain made of ice and salt that erupted relatively recently. The discovery reveals that small worlds can retain subsurface oceans and geological activity far longer than expected, expanding the range of potentially habitable environments in our solar system.

Scientists discovered 24-hour protein rhythms in cells without DNA, revealing an ancient timekeeping mechanism that predates gene-based clocks by billions of years and exists across all life.
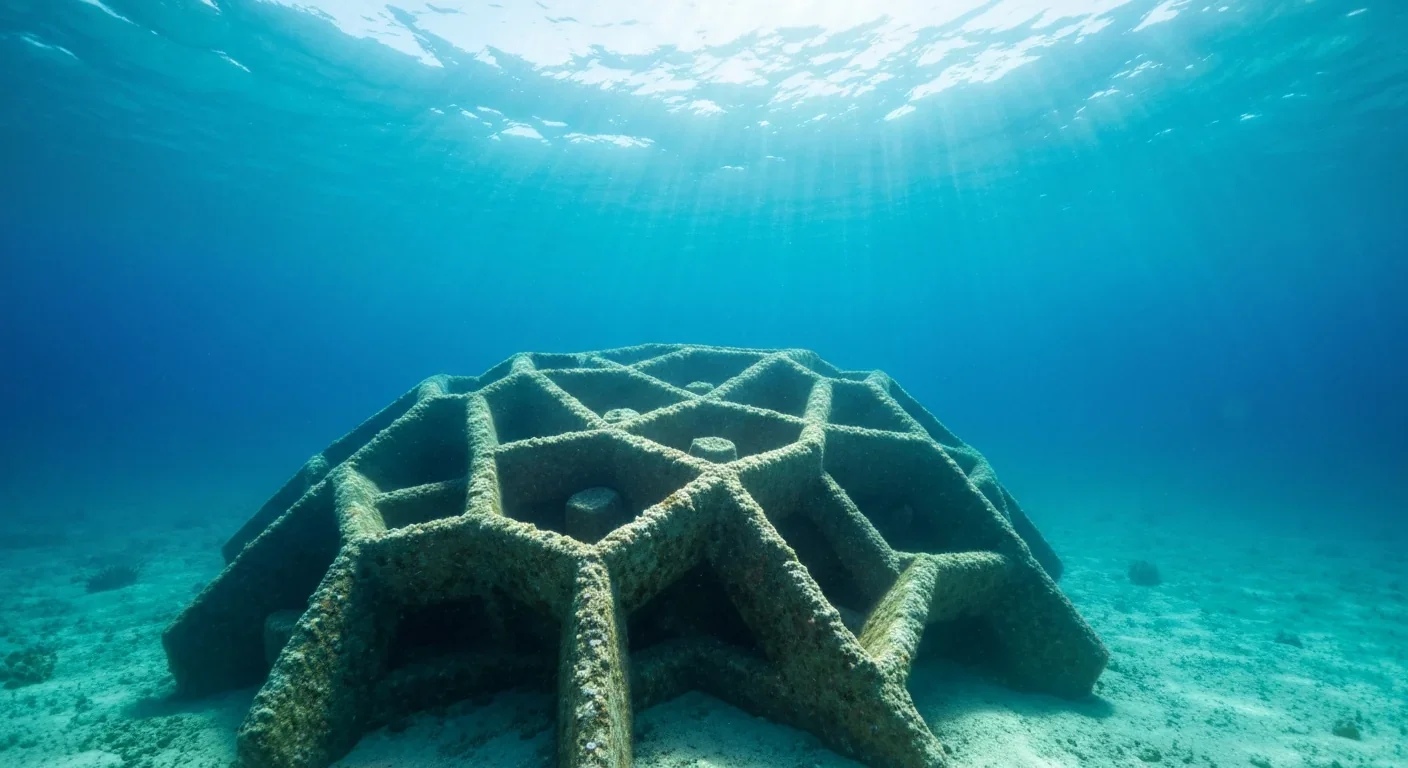
3D-printed coral reefs are being engineered with precise surface textures, material chemistry, and geometric complexity to optimize coral larvae settlement. While early projects show promise - with some designs achieving 80x higher settlement rates - scalability, cost, and the overriding challenge of climate change remain critical obstacles.

The minimal group paradigm shows humans discriminate based on meaningless group labels - like coin flips or shirt colors - revealing that tribalism is hardwired into our brains. Understanding this automatic bias is the first step toward managing it.
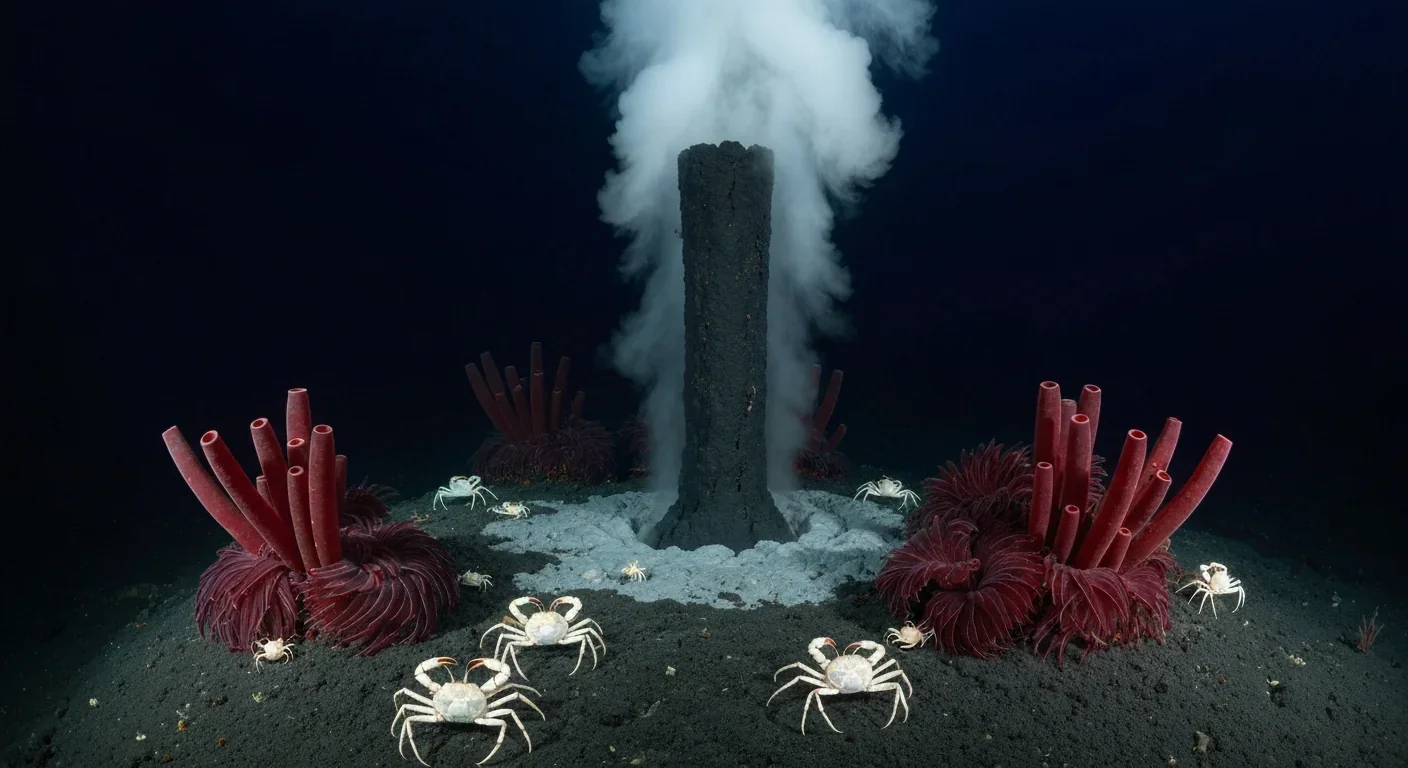
In 1977, scientists discovered thriving ecosystems around underwater volcanic vents powered by chemistry, not sunlight. These alien worlds host bizarre creatures and heat-loving microbes, revolutionizing our understanding of where life can exist on Earth and beyond.

Automated systems in housing - mortgage lending, tenant screening, appraisals, and insurance - systematically discriminate against communities of color by using proxy variables like ZIP codes and credit scores that encode historical racism. While the Fair Housing Act outlawed explicit redlining decades ago, machine learning models trained on biased data reproduce the same patterns at scale. Solutions exist - algorithmic auditing, fairness-aware design, regulatory reform - but require prioritizing equ...
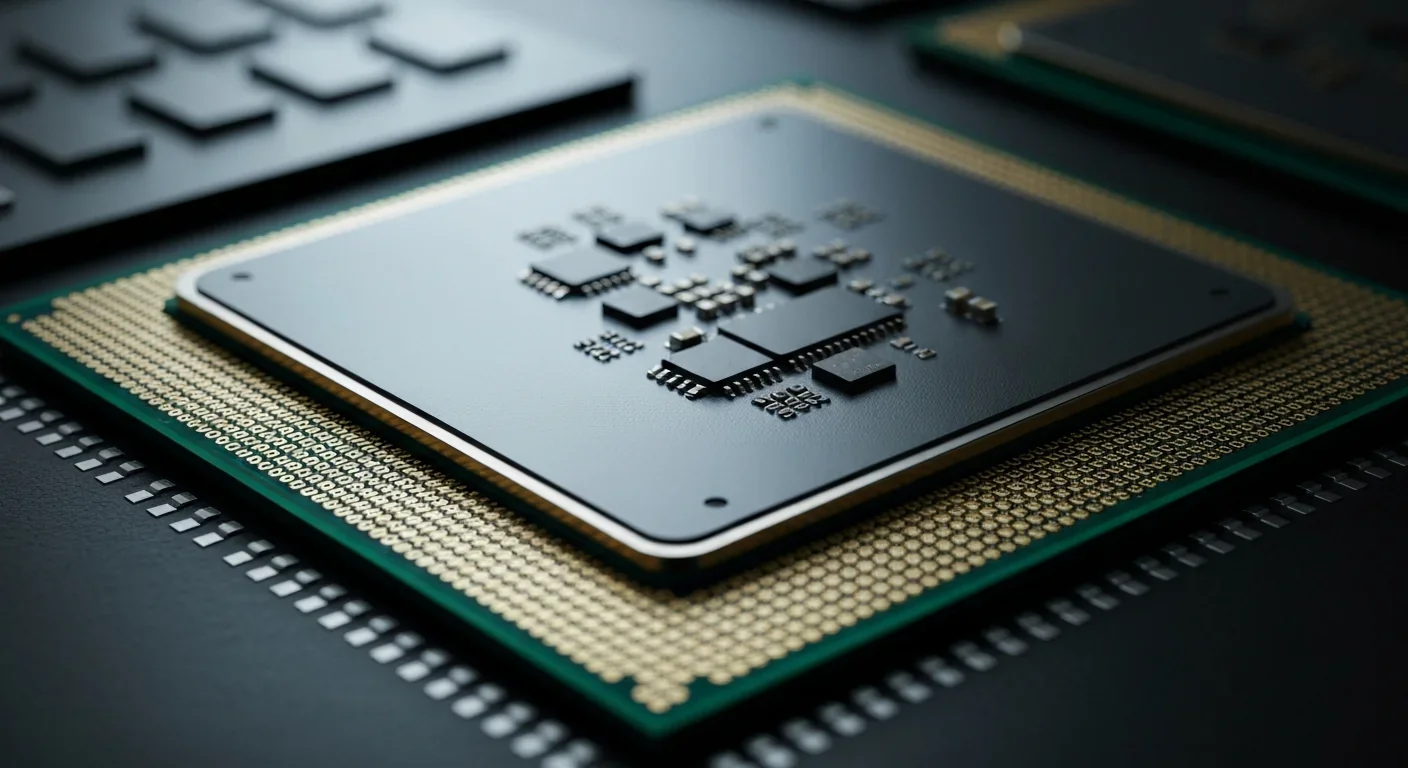
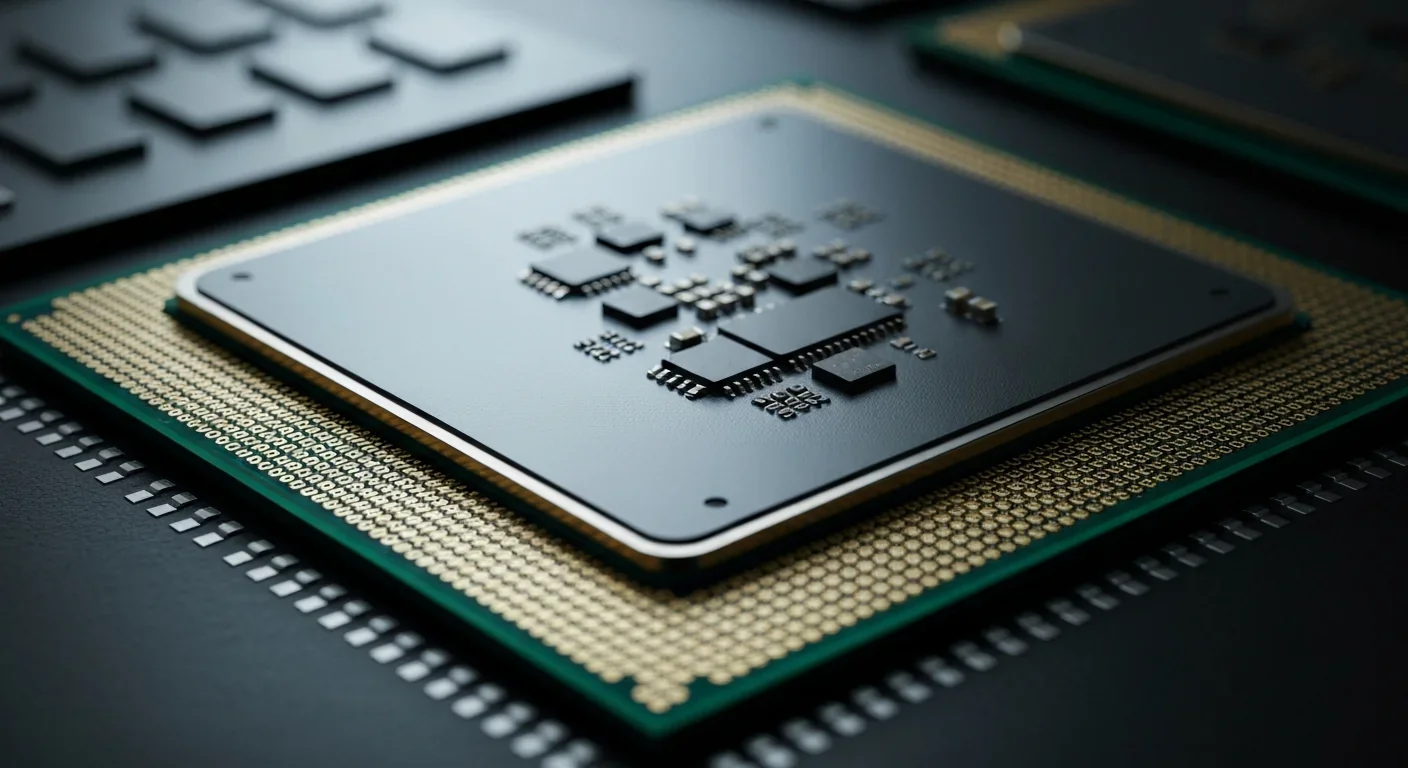
Cache coherence protocols like MESI and MOESI coordinate billions of operations per second to ensure data consistency across multi-core processors. Understanding these invisible hardware mechanisms helps developers write faster parallel code and avoid performance pitfalls.